Richard Yocum, MD, San Diego Mountain Rescue Team and Riverside Mountain Rescue Unit
Frostbite is a painful condition often resulting in loss of tissue that is usually preventable. The Wilderness Medical Society (WMS) published a 2019 update to their clinical practice guidelines for the prevention and treatment of frostbite1 , which serves as the primary basis for this discussion along with research by Cauchy et al. in Chamonix, France.2,3 Frostnip and frostbite occur when heat loss exceeds the ability of blood flow to deliver heat to tissues and prevent freezing.
Preventive Measures
• Avoid/minimize duration of exposure to extreme cold conditions, especially wet and high wind-chill
• Maintain adequate hydration and caloric intake
• Maintain adequate core temperature
• Cover all skin/scalp to protect from cold, wind, and moisture
• Use multiple clothing layers including wind protection
• Change from gloves to mittens
• Minimize blood flow restriction from constrictive clothing/footwear and inactivity
• Avoid perspiration and wet extremities
• Consider exercise to increase blood flow to the periphery (unless there is risk of exhaustion)
• Consider warmth from adjacent body heat, such as patient’s own armpit or abdomen
• Consider chemical or electrical warmers for hands/feet
• Minimize effects of known diseases, medications, and substances (alcohol, drugs, tobacco)
• Regularly check all members in group for early signs of frostnip/frostbite
• Recognize early and treat immediately cold-induced numbness/frostnip
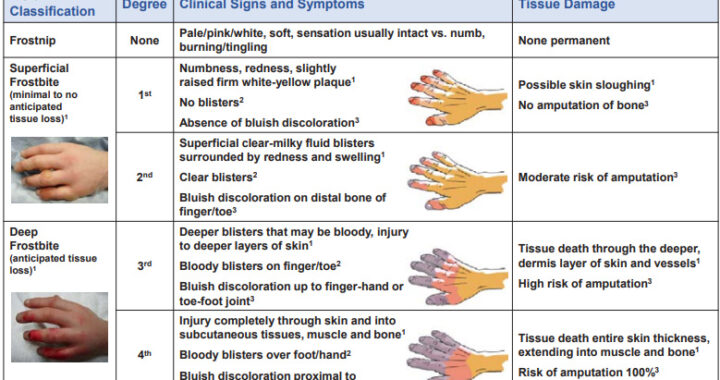
Frostnip is a superficial cold injury distinct from frostbite but may precede frostbite. Although frostnip resolves with rewarming without permanent tissue damage, frostnip signals that appropriate action is immediately needed to prevent frostbite. Frostbite is traditionally categorized into 4 grades of severity of tissue damage based on clinical findings immediately after rewarming. Because these distinctions are difficult to assess before rewarming, a 2-tiered classification of superficial vs. deep is more appropriate for the field. A given patient may present with frostbite in more than one location with varying grades of severity.
Some treatment recommendations may be generalized to most cases of frostbite.
Treatment General to All Frostbite
• Remove jewelry/other constrictive material from affected body part
• Assure adequate hydration and caloric intake
• Treat any underlying hypothermia (if mild, treat concurrently with frostbite; if moderate-
severe, treat before treating frostbite)
• Start ibuprofen at a dose of 12 mg/kg divided twice daily to maximum 2400 mg/day in 4
divided doses (e.g., for 70 kg patient, 400 mg twice daily to 600 mg 4 times daily)
(Nonsteroidal drugs such as ibuprofen can reduce vasoconstriction and tissue damage)
• If available, supplemental oxygen if hypoxic (O2 sat < 88% or elevation > 4000 m/13,000’)
• Do not debride/open blisters in the field
• Do not rub/apply ice or snow
Criteria for Field Rewarming
• No chance of refreezing
• Definitive care > 2 hours distant
• Ability/equipment available to thaw
The most important decision is whether to thaw frozen tissue in the field. Refreezing is devastating. If there is a risk of thawed tissue refreezing, do not thaw; keep the affected tissue frozen until a thawed state can be maintained, such when out of the field. However, tissue should not be intentionally kept frozen if environmental conditions allow for spontaneous thawing; frozen tissue should be allowed to thaw. Active rapid warming is preferred over slow passive warming. Rewarming in the field should adhere to clinical practice guidelines and anticipate the need to manage significant pain.
How to Rewarm in the Field
• Use warm (not hot) water bath (37-39 C, 98.6-102.2 F, verified to be tolerated by noninjured hand ≥ 30
seconds) immersion for rapid rewarming until tissue is soft and pliable to touch, then air dry (don’t rub).
Avoid risk of thermal burns from fire, heated rocks, etc.
• Apply bulky, clean, loosely-wrapped, dry gauze/cotton dressings over thawed part/between fingers/toes
• Topical aloe vera may be applied to thawed tissue before dressing
• Nonsteroidal drug (e.g., ibuprofen) or opiate analgesic as needed for pain control
• Protect from refreezing and further trauma
• If possible, elevate the thawed extremity to reduce swelling
• Avoid use of thawed part if possible
If frostbite does not meet criteria for field rewarming, field treatment is directed at preventing further injury from trauma. Bulky dressings may be applied as described above for rewarmed frostbite.
A risk-benefit analysis may be required before using a frozen or thawed body part for ambulation. If avoidable, a frozen extremity should not be used for walking, climbing, etc.; however, it may be reasonable for evacuation purposes to walk on frozen toes or feet and on thawed toes, but inadvisable to walk on an entire foot that has been thawed.
Awareness of these preventive measures and guidelines may prevent permanent damage and the painful loss of body tissue.
[Click to view larger image – here’s the text: ]
Field Classification Degree Clinical Signs and Symptoms Tissue Damage Frostnip None Pale/pink/white, soft, sensation usually intact vs. numb, burning/tingling None permanent Superficial Frostbite (minimal to no anticipated tissue loss)1 1st Numbness, redness, slightly raised firm white-yellow plaque1 No blisters2 Absence of bluish discoloration3 Possible skin sloughing1 No amputation of bone3 2nd Superficial clear-milky fluid blisters surrounded by redness and swelling1 Clear blisters2 Bluish discoloration on distal bone of finger/toe3 Moderate risk of amputation3 Deep Frostbite (anticipated tissue loss)1 3rd Deeper blisters that may be bloody, injury to deeper layers of skin1 Bloody blisters on finger/toe2 Bluish discoloration up to finger-hand or toe-foot joint3 Tissue death through the deeper, dermis layer of skin and vessels1 High risk of amputation3 4th Injury completely through skin and into subcutaneous tissues, muscle and bone1 Bloody blisters over foot/hand2 Bluish discoloration proximal to finger-hand or toe-foot joint3 Tissue death entire skin thickness, extending into muscle and bone1 Risk of amputation 100%3 Treatment General to All Frostbite • Remove jewelry/other constrictive material from affected body part •
1. McIntosh SE, Freer L, Grissom CK, Auerbach PS, Rodway GW, Cochran A, et al. Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Frostbite: 2019 Update, Wilderness & Environmental Medicine 2019;30(4S):S19-S32. 2. Cauchy E, Chetaillle E, Marchand V, Marsigny G. Retrospective Study of 70 Cases of Severe Frostbite Lesions: A Proposed New Classification Scheme, Wilderness & Environmental Medicine 2001;12:248-255. 3. Cauchy E, Davis CB, Pasquier M, Meyer EF, Hackett PH. A New Proposal for Management of Severe Frostbite in the Austere Environment, Wilderness & Environmental Medicine 2016;27:92-99.